
IBS Explained: What It Is and How GPs Can Help
Learn what IBS is, common symptoms, possible causes, and how Australians can access GP and telehealth support for ongoing care.


Learn what IBS is, common symptoms, possible causes, and how Australians can access GP and telehealth support for ongoing care.

Learn when yeast infections can be treated through online prescriptions in Australia, including who is eligible, available treatments, and when to see a doctor.

Explore finasteride’s mental health risks, compare minoxidilfinasteride side effects, and discover regulators’ approach to finasteride for hair loss.

Learn if pensioners still get bulkbilled telehealth, how to claim it, and which Australian providers offer free virtual GP visits for concession cardholders.
Find out when Australians may be eligible for a medical certificate for insomnia, how to request one online, and what your employer can and cannot ask for.
Learn how herpes can be managed through telehealth in Australia, including online consultations, treatment options, and ongoing care support.
Explore online depression treatment in Australia: how it’s diagnosed, telehealth tiers for mildtosevere cases, Medicare rebates and the new 2026 digital service.
Discover how Telehealth services in Australia can provide access to ED medications. Learn about online consultations and online prescriptions for discreet treatment.
Learn how Australian students can obtain a medical certificate for study or exam absences, including online options, university requirements, and eligibility.
We provide clear, practical guidance to help you understand and compare GP services. The services that we recommend will help you compare online clinics and ultimately choose the right one for your needs.

Learn what IBS is, common symptoms, possible causes, and how Australians can access GP and telehealth support for ongoing care.

Learn more about what to do when you’re sick and your doctor isn’t available. Telehealth, comparison platforms and their purpose in Australian healthcare.

Discover how choosing the right telehealth provider instead of delaying GP visits can help you manage your health, improve outcomes, and save you money.
The sexual health guides cover key issues as well as available testing and treatment options offered by online telehealth professionals. We also provide information about the expected experience during a visit, the average cost, and how to choose the right provider.

Learn how herpes can be managed through telehealth in Australia, including online consultations, treatment options, and ongoing care support.

Discover how Telehealth services in Australia can provide access to ED medications. Learn about online consultations and online prescriptions for discreet treatment.
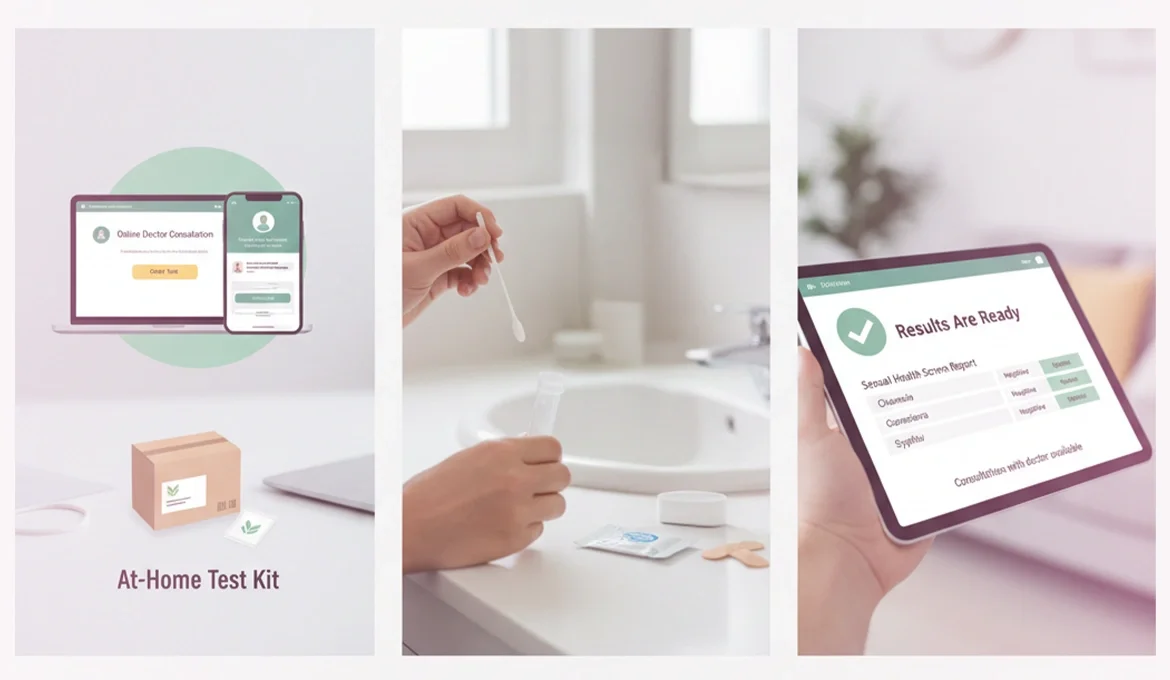
Learn stepbystep how online STI testing works, the providers, pricing, turnaround times and privacy benefits for Australian patients.
Medicompare’s mental health articles offer practical guidance on addressing common mental health concerns in Australia. If you’re looking to improve your mental health, we are here to help with useful information via our blog.

Explore finasteride’s mental health risks, compare minoxidilfinasteride side effects, and discover regulators’ approach to finasteride for hair loss.

Learn how online mentalhealth screening works in Australia, the steps to obtain a Medicaresubsidised treatment plan, and what to expect from your telehealth GP visit.

Learn practical steps Australians can take to book a same‑day telehealth anxiety appointment, including how to compare trusted platforms and stay safe online.
Here, you’ll find straightforward explanations of eligibility and billing for Bulk Billed services. Compare options online and learn what’s included before you book with a provider.

Learn if pensioners still get bulkbilled telehealth, how to claim it, and which Australian providers offer free virtual GP visits for concession cardholders.

Learn which GP telehealth services are bulkbilled, including after-hours consults and telehealth for infants, and how to find free bulk billing providers.

On-demand telehealth may still request your Medicare or IHI number for identity checks, medical records and e-prescribing—not to claim Medicare rebates.
These articles compare weight loss programs to help you choose the right provider. At Medicompare, we help you compare the top providers and give you the best advice possible.

Explore online depression treatment in Australia: how it’s diagnosed, telehealth tiers for mildtosevere cases, Medicare rebates and the new 2026 digital service.
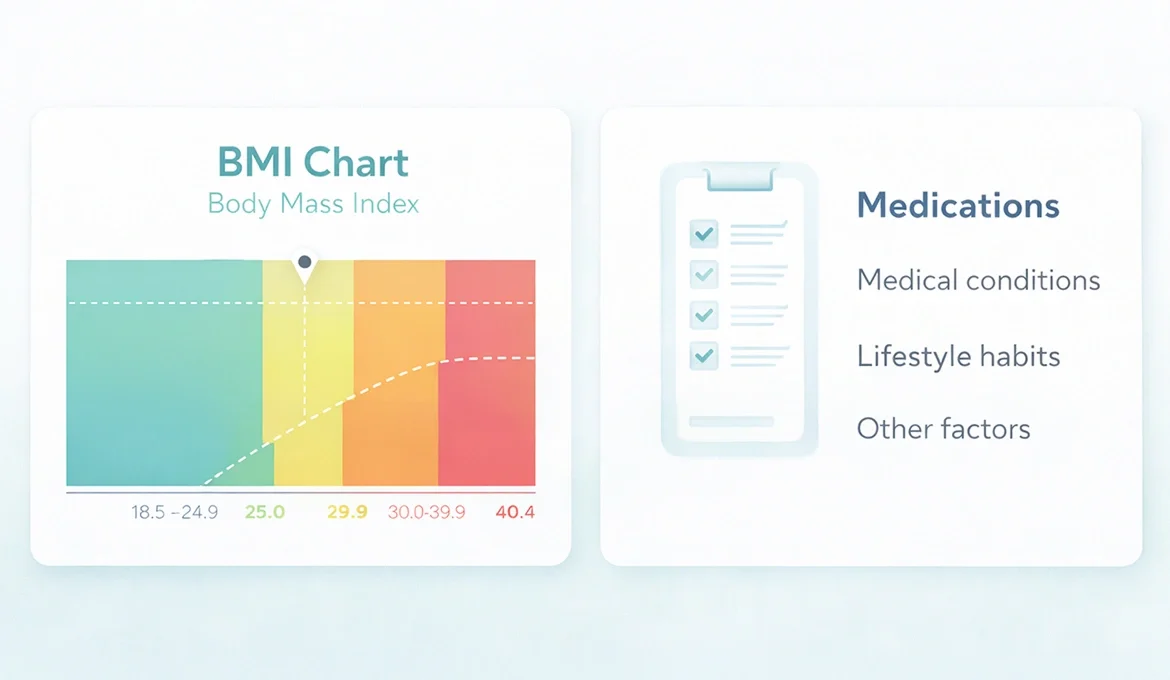
MediCompare’s patient guide to why telehealth providers use BMI, how they assess your medical history, how to check BMI online, and Aussie rules for weight loss meds.

Considering overseas providers for weight loss or ketamine therapy? Discover why Aussie telehealth beats other options, plus trusted providers, costs, safety tips and TGA rules explained.
Our hair loss articles outline the main treatment pathways for common hair loss conditions. We compare hair loss providers and review Australian programs that are currently available on the market.

Explore finasteride’s mental health risks, compare minoxidilfinasteride side effects, and discover regulators’ approach to finasteride for hair loss.

Explore whether finasteride is a long-term solution for hair loss, including its effectiveness, side effects, and alternatives.

Discover discreet, personalised hair loss treatments via telehealth in Australia, with AHPRA-registered doctors and holistic care options.
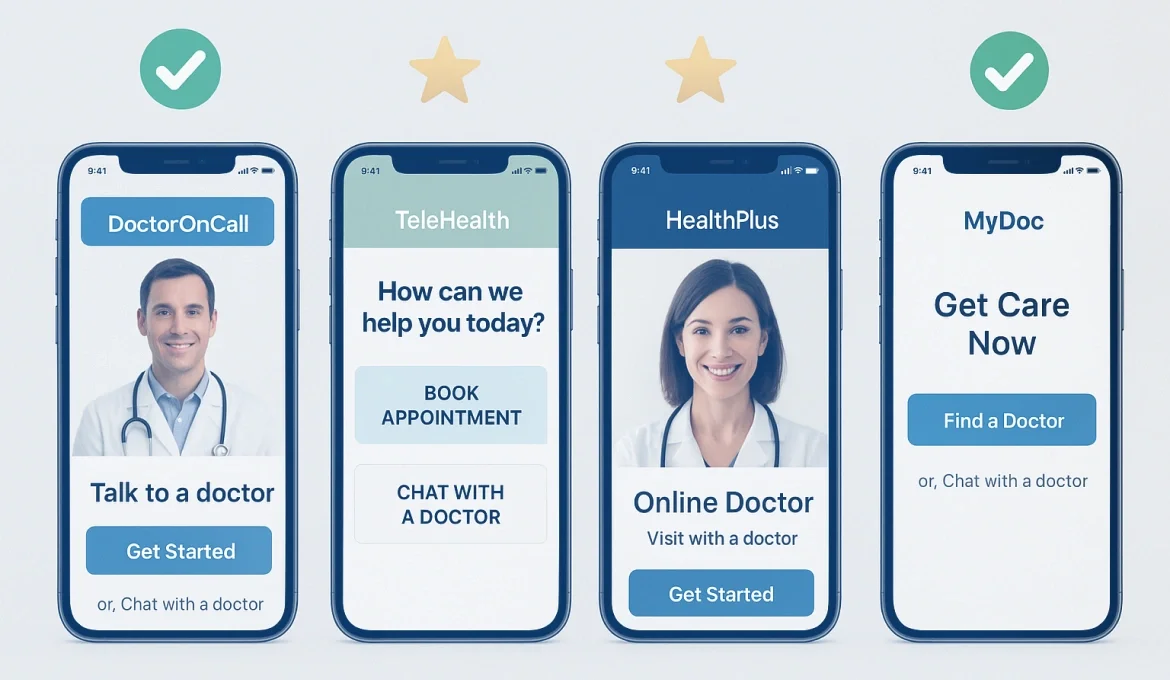
Medicompare’s comprehensive guide to Australia’s mostused online doctor apps, covering services, cost, user experience, privacy and clinician credentials.

Find safe, affordable telehealth for kids, teens and elderly parents in 2026. Compare cost, paediatric expertise, wait times and medication delivery.

Explore how family-focused telehealth in Australia offers convenient after-hours care, Medicare bulkbilling, and trusted providers for kids and parents.
Tal, a father of two high-energy boys, and a trained Australian physician, believes in an interconnected healthcare future, where knowledge is accessible everywhere, where consumers are truly centric to health, where data is interpreted for actionable insights, where patients are treated bespokely as people, and where health innovations focus on the triple aim – better health outcomes, healthcare efficiencies, and improved customer experience of health.
Kiara is a registered nurse and nurse educator, having worked in the industry for over 10 years. In the last couple of years, she has begun utilising her clinical experience to write healthcare content that is informative and relevant. Outside of work Kiara enjoys being outdoors in nature, gardening, cooking, and spending time with friends and family.
Nethel has a passion for the health industry, having worked in two countries as both a pharmacist and nurse. She is dedicated to providing safe, holistic and evidence-based information for her readers.
Anna is a skilled content creator specializing in wellness, health, and lifestyle topics. In over 20 years of working as acreative, she has crafted engaging online and print content, starting as a newsroom journalist and evolving into a writer and editor for lifestyle and health magazines and websites. Her diverse portfolio also includes blogging, scripting for YouTube, ghostwriting books and thought leadership articles, and working as a columnist.
📍Bondi, NSW, Australia, 2026
Medicompare pty Ltd is an independent review platform and is not affiliated with or endorsed by any government agency or Medicare.
Trademarks, logos, and product names are the property of their respective owners. Use of these marks does not imply endorsement.